NAPLES, FLORIDA TOP PROLIFIC LYME AUTHOR: ANOTHER DISCOVERY — LL MD BLIND SPOT? LONG-TERM PARTICLES
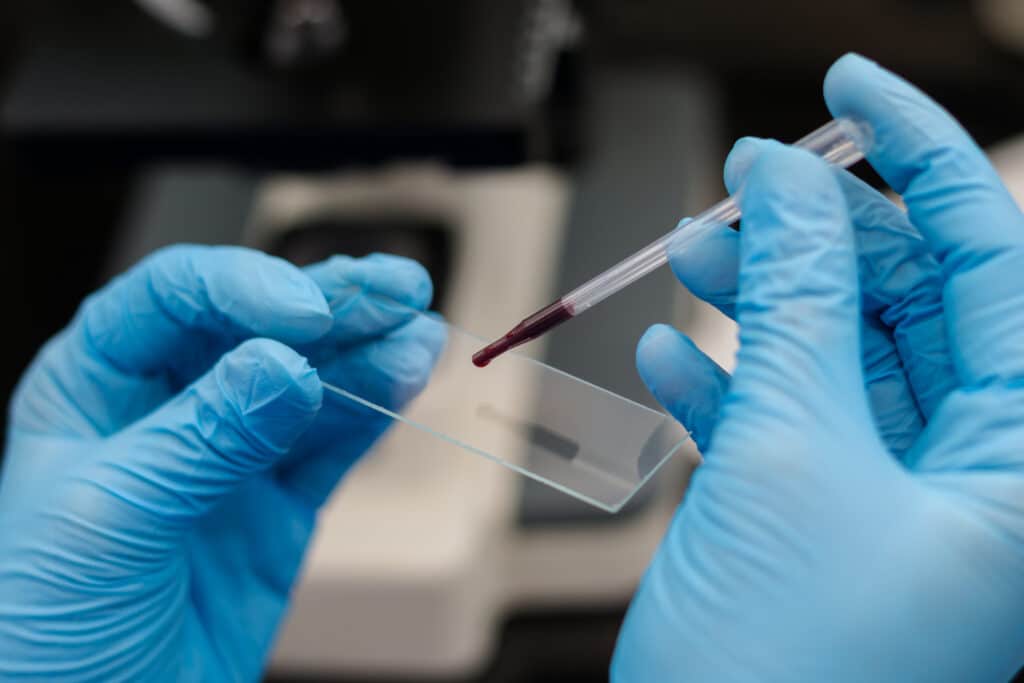
My Friend Ray Stricker reminded me of the Body’s Great Clean-up System. Amazing. So I thought I could not overwhelm the body’s enzymes and other clean-up tools with immense TBD particles, fragments, or “unruly debris.” This is not a mere “herx.” And then I was far too aggressive with some hyper alpha types, who profoundly […]