FLORIDA PHYSICIAN EXPLAINS IF YOU LEARN ABOUT “LEAKY GUT” LOOK AT INTESTINAL PERMEABILITY RESEARCH.
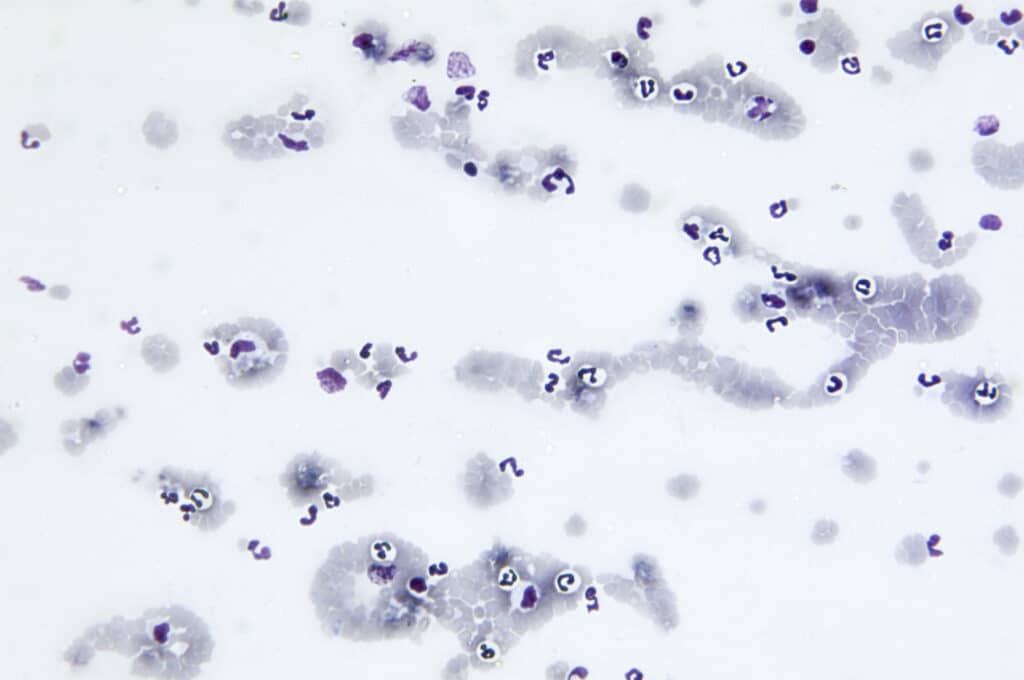
Review Am J Physiol Gastrointest Liver Physiol . 2020 Nov 1;319(5):G589-G608. doi: 10.1152/ajpgi.00245.2020. Epub 2020 Sep 9. Effects of dietary components on intestinal permeability in health and disease Katayoun Khoshbin 1, Michael Camilleri 1 Affiliations expand PMID: 32902315 PMCID: PMC8087346 DOI: 10.1152/ajpgi.00245.2020 Abstract Altered intestinal permeability plays a role in many pathological conditions. Intestinal permeability […]